
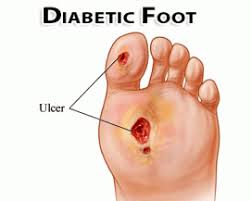
Patients with diabetes mellitus frequently develop chronic wounds as a result of impaired wound healing. This has negative effects for both the patient and the medical system, and with the rising prevalence of diabetes, it will soon become a major medical, social, and economic burden. As a result, therapeutic alternatives to the currently available treatments, which, while diverse, do not guarantee a rapid and complete healing process, seemed to be necessary.
In diabetes, a complicated pathophysiology comprising vascular, neuropathic, immunological, and metabolic components leads to impaired repair Hyperglycemia is linked to stiffer blood arteries, which result in slower circulation and microvascular dysfunction, resulting in decreased tissue oxygenation. Diabetic patients' blood vessel changes also result in less leukocyte migration into the wound, making it more susceptible to infection. Leucocyte function can be harmed by the hyperglycemic environment. Peripheral neuropathy can also cause numbness and a reduced ability to sense pain, which can contribute to the chronicization of infections that aren't appropriately treated right away